Forensic Toxicology Services
Scientific Expertise for the Legal Community
About FTS

Forensic Toxicology Services
(FTS) is a scientific resource for the legal community in the areas of forensic toxicological analysis and interpretation. FTS is no longer accepting casework or providing consultation services but remains available for educational activities. Professional referral is available. FTS is located in Birmingham, AL.
Contact an Expert
Toxicology
is the study of drugs and poisons and their effects on the health and/or performance of the consumer.

Forensic Toxicology
is the application of toxicological principles to medical-legal issues such as cause and manner of death and subject performance or behavior relating to criminal and other regulated activity.

Toxicological Testing
is a laboratory-based process whereby specimens are examined for substances of toxicological significance (drugs, alcohols, poisons). Test findings based upon proficient laboratory analyses are scientifically accurate and reliable. Variables such as, but not limited to specimen source, collection, timing, custody, maintenance, availability and condition do not effect scientific accuracy and reliability unless they disrupt the testing process.
It is what it is.
Read More
Toxicological Interpretation
is a post-testing, non-laboratory process whereby the significance of test findings is examined in relation to the context of the case. Variables such as, but not limited to specimen source, collection, timing, custody, maintenance, availability and condition can affect the interpretation of otherwise scientifically accurate and reliable test findings.
But it could mean something else.
Read More
Expertise
Pain, Prison, Postmortems
I see humanity ease melancholy with insobriety
Gluttony unleash revelry, calamity, tragedy
Addiction, infirmity, need for remedy
Reality, finality, a bag for everybody
Pain, prison, postmortems
Misery run deep
I atone with all sincerity
Imply no indignity
Cope with levity
Lest I weep

A... as in apple autopsy
"This was the most unkindest cut of all"
- Marcus Antonius/William Shakespeare
"Helping neighbor look for gas leak under his trailer
Lit match to detect gas leak
BOOM
Refused medical attention
Later showed up at hospital complaining of burns
Autopsy"

"You know I've smoked a lot of grass
O' Lord, I've popped a lot of pills
But I never touched nothin'
That my spirit could kill"
- Hoyt Axton/Steppenwolf
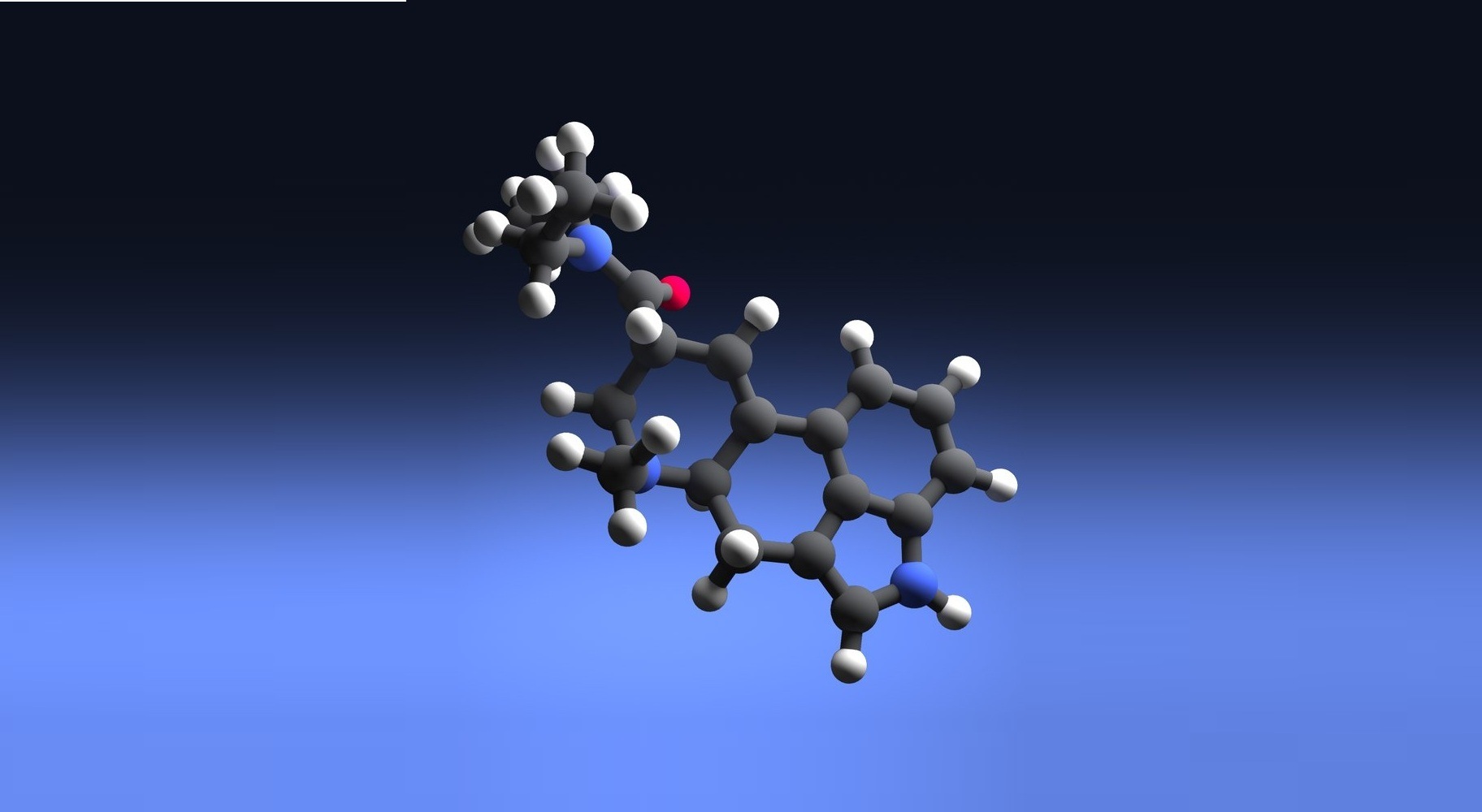
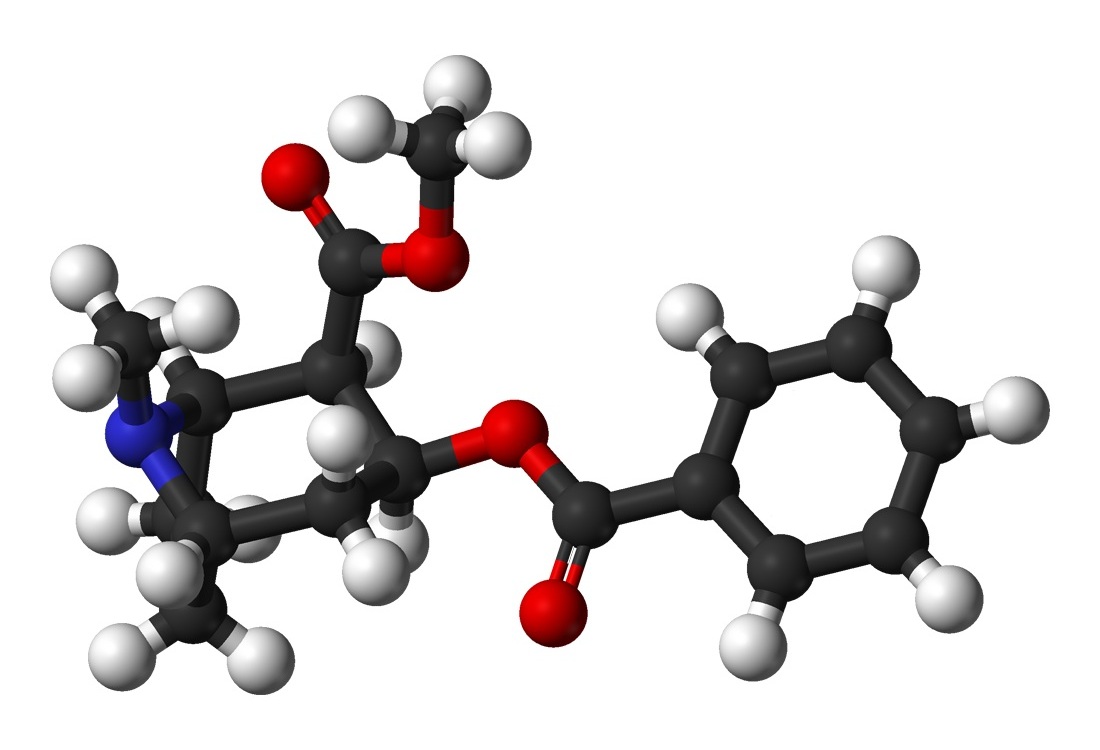
A scientist's view of morphine
"I've seen the needle and the damage done
A little part of it in everyone
But every junkie's like a settin' sun"
- Neil Young
"One pill makes you larger
And one pill makes you small
And the ones that mother gives you
Don't do anything at all
Go ask Alice
When she's ten feet tall"
- Jefferson Airplane

These don't come with warnings
"If you wanna hang out
You've got to take her out
Cocaine
If you wanna get down
Down on the ground
Cocaine
She don't lie
She don't lie
She don't lie
Cocaine"
- John Cale/Eric Clapton
"Gramma gets that way on crack"
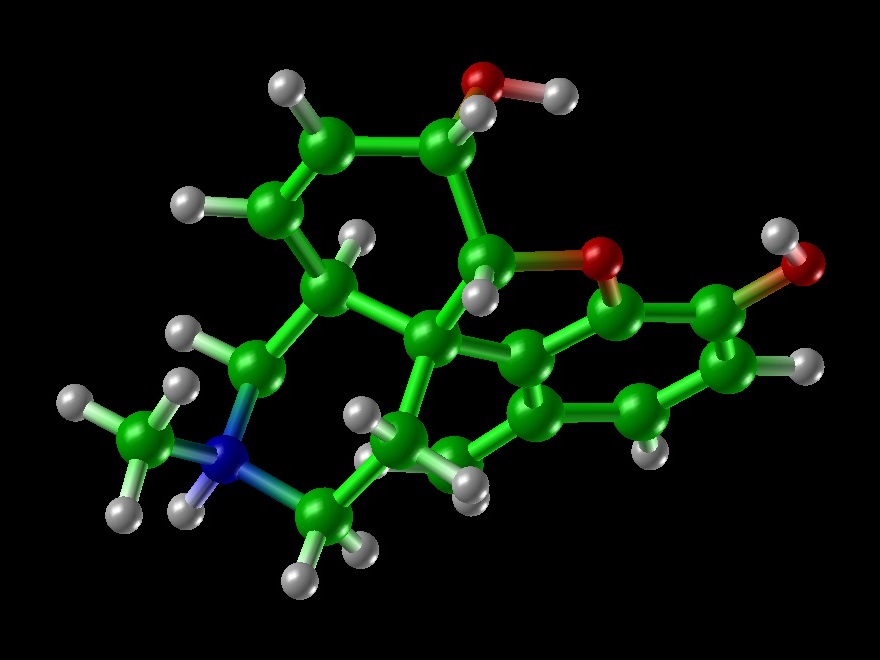
A scientist's view of cocaine
"I'm your mama, I'm your daddy
I'm that n**** in the alley
I'm your doctor when in need
Want some coke? Have some weed
You know me, I'm your friend
Your main boy, thick and thin
I'm your pusherman
I'm your pusherman"
- Curtis Mayfield
"Driving that train, high on cocaine
Casey Jones you better watch your speed
Trouble ahead, trouble behind
And you know that notion just crossed my mind"
- Grateful Dead

"Perhaps you’d understand it better
Standin’ in my shoes
It’s the ultimate enticement
It’s the smuggler’s blues
It’s a losing proposition
But one you can’t refuse
It’s the politics of contraband
It’s the smugglers blues"
- Glenn Frye
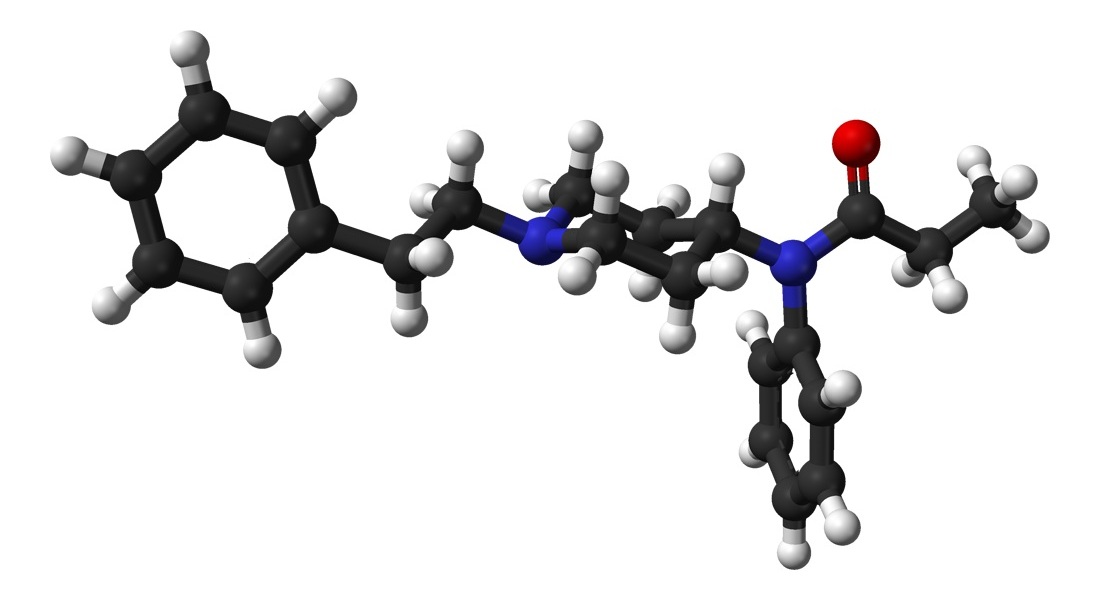
A scientist's view of fentanyl
"Oh, I get by with a little help from my friends
Mm, I get high with a little help from my friends
Mm, gonna try with a little help from my friends"
- Joe Cocker/Beatles
You can die with a little help from your friends

Say hello to my friends
"Well, my baby, she gone, gone tonight
I ain't seen the girl since night before last
I wanna get drunk, get off of my mind
One bourbon, one scotch, and one beer"
- Amos Milburn
- John Lee Hooker
- George Thorogood/The Destroyers

Judge: Looks here like you were drinkin’
Defendant: No, I was fishin’
Judge: What do you do when you go fishin’?
Defendant: I cool off with beer
Judge: I call that drinkin’
Defendant: Nope, drinkin's when you’re in a bar

A first responder's view of ethanol

"Pour me somethin' tall an' strong
Make it a "Hurricane" before I go insane
It's only half-past twelve but I don't care
It's five o'clock somewhere"
- Alan Jackson

We're not supposed to drink and drive
Yet we have beer-branded key rings
"Oh, show me the way to the next whiskey bar
Oh, don't ask why, no, don't ask why
For we must find the next whiskey bar
Or if we don't find the next whiskey bar
I tell you we must die, I tell you we must die
I tell you, I tell you, I tell you we must die"
- The Doors
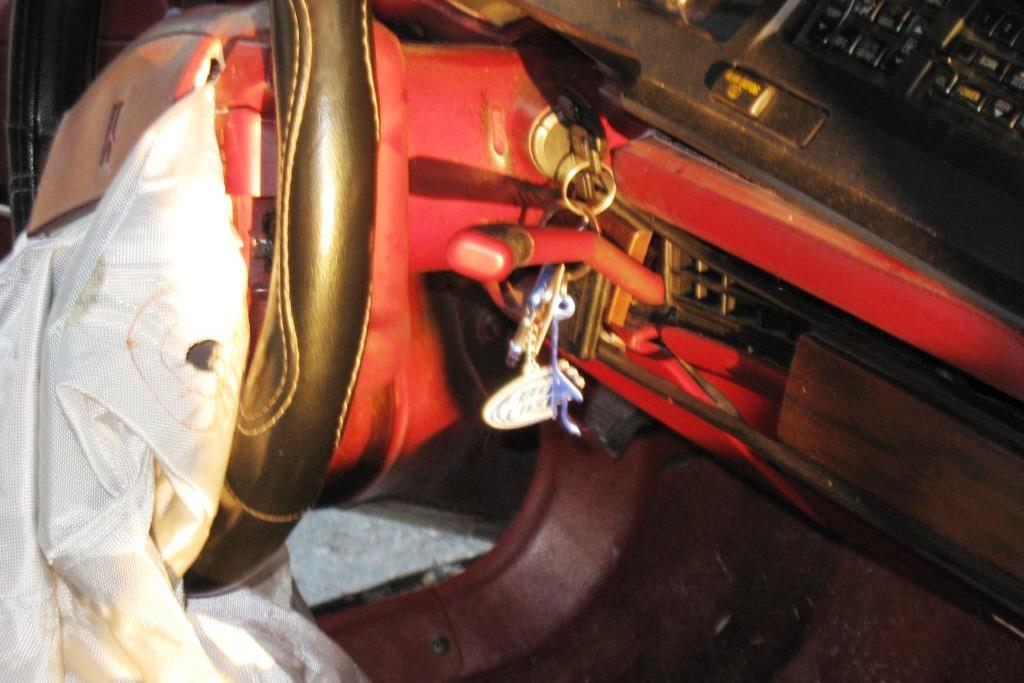
We're not supposed to drink and drive
Yet we have bottle opener key rings
"It's nine o'clock on a Saturday
The regular crowd shuffles in
There's an old man sittin' next to me
Makin' love to his tonic and gin
And the waitress is practicing politics
As the businessmen slowly get stoned
Yes, they're sharing a drink they call loneliness
But it's better than drinkin' alone"
- Billy Joel
"I ain't as good as I once was
That's just the cold hard truth
I still throw a few back, talk a little smack
When I'm feelin' bullet proof
So don't double dog dare me now
'Cause I'd have to call your bluff
I ain't as good as I once was
But I'm as good once as I ever was.
May not be good as I once was
But I'm as good once as I ever was."
- Toby Keith

"I'll learn to work the saxophone
I'll play just what I feel
Drink Scotch whiskey all night long
And die behind the wheel
They got a name for the winners in the world
I'll want a name when I lose
They call Alabama the Crimson Tide
Call me Deacon Blues"
- Steely Dan
"It's a tough ol' life up here on the wagon
I'm feedin' the dog, sackin' the trash
It's honey do this honey do that
I sobered up, and I got to thinkin'
Girl you ain't much fun since I quit drinkin'
Yeah I sobered up, and I got to thinkin'
Girl you ain't much fun since I quit drinkin'"
- more Toby Keith

"I blew out my flip-flop, stepped on a pop top
Cut my heel, had to cruise on back home
But there's booze in the blender
And soon it will render
That frozen concoction that helps me hang on
Wastin' away in Maragaritaville..."
- Jimmy Buffet

"I love this bar
It's my kind of place
Just walkin' through the front door
Puts a big smile on my face
It ain't too far, come as you are...
And we like to drink our beer from a mason jar
Hmmm, hmmm, hmmm, hmmm, hmmm I love this bar"
- more Toby Keith
"All week long we're some real nobodies
But we just punched out, it's paycheck Friday
Weekend's here, good God almighty
People let's get drunk and be somebody"
- more Toby Keith
"No, no, no, no, I don't (sniff) it no more
I'm tired of waking up on the floor
No, thank you, please
It only makes me sneeze
Then it makes it hard to find the door"
- Hoyt Axton/Ringo Starr

What's it gonna be?
[Sniff] Hit me again.
[Sniff] And one for my friend.

"And here, she's acting happy
Inside her handsome home
And me, I’m flying in my taxi
Taking tips, and getting stoned
I go flying so high, when I’m stoned"
- Harry Chapin

"Don't bogart that joint my friend
Pass it over to me"
- Fraternity of Man

A scientist's view of THC
"One toke over the line, sweet Jesus
One toke over the line
Sitting downtown in a railway station
One toke over the line"
- Brewer and Shipley
- Lawrence Welk
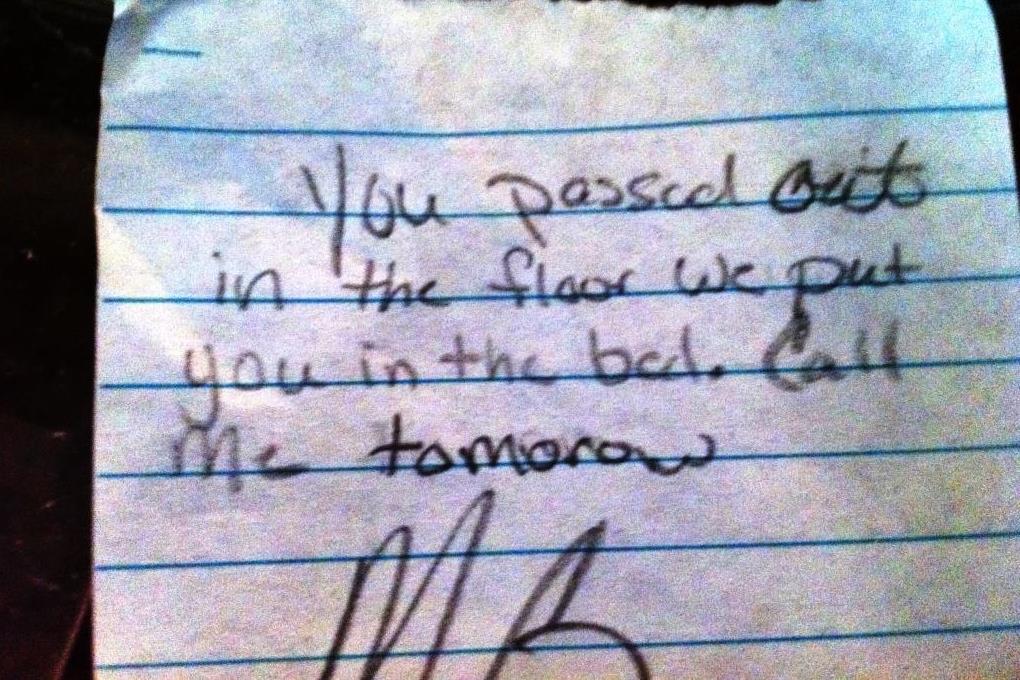
"Some radio is blastin'
Someone's knockin' at the door
I'm lookin' at my girlfriend
She passed out on the floor
I've seen so many things
I ain't never seen before
Don't know what it is
I don't wanna see no more"
- Randy Newman
- Three Dog Night

"Think I'll spend eternity in the city
Let the carbon and monoxide choke my thoughts away, yeah
And pretty bodies help dissolve the memories
They can never be what she was (was) to (to) me"
- Hall and Oates

"Every night I go to sleep
The blues fall down like rain
Taking pills, cheap whiskey
Just to try to ease the pain"
- Blues Brothers
"Well, I woke up this mornin'
And I got myself a beer
Well, I woke up this mornin'
And I got myself a beer
The future's uncertain
And the end is always near"
- more Doors